(517) 487-5171
Fax (517) 908-0172

What is a Podiatrist?
The branch of medicine that is focused on the treatment, diagnosis, and study of disorders of the lower leg, ankle and foot is referred to as podiatry. Because people often spend a great deal of their time on their feet, many problems in this area can occur. A person seeks help from the field of podiatry when they need treatment for heel spurs, bunions, arch problems, deformities, ingrown toenails, corns, foot and ankle problems, infections, and problems with the foot that are related to diabetes and additional diseases.
To treat problems of the foot, ankle or lower leg, a podiatrist may prescribe physical therapy, drugs, perform surgery, or set fractures. Individuals may also be recommended to wear corrective shoe inserts, custom-made shoes, plaster casts and strappings in order to correct deformities.
When trying to gather information on a patient problem, a scanner or force plate may be used in order to design orthotics. During this procedure, patients are told to walk across a plate that is connected to a computer; the computer then takes a scan of the foot and indicates weight distribution and pressure points. The computer readouts will give the podiatrist information to help them determine the correct treatment plans.
Diagnosis is also provided through laboratory tests and x-rays. Through the foot, the first signs of serious problems such as heart disease, diabetes and arthritis can show up. For example, individuals that have diabetes may frequently have problems such as infections and foot ulcers because they experience poor circulation in the foot area. A podiatrist can then have consultations with patients when symptoms arise. Referrals will then be made to specialists that handle the greater health problems.
Some podiatrists have their own independent, private practices or clinics where they have a small staff and administrative personnel. Many podiatrists work within group practices. They usually spend time performing surgery in ambulatory surgical centers or hospitals, or visit patients in nursing homes. Podiatrists typically spend between 30 to 60 hours of week working. Some podiatrists specialize in public health, orthopedics, surgery, or primary care. Other fields include specialties in geriatrics, dermatology, pediatrics, diabetic foot care and sports medicine.
Some podiatrist specialists complete extra training in the area of foot and ankle reconstruction that results from the effects of physical trauma or diabetes. There are also surgeons that perform surgery of a cosmetic nature to correct bunions and hammertoes.
Why Are Biomechanics of the Foot Important to Older Adults?
 As we age, biomechanics—the study of structure, function and movement—become more important to our foot health. Aging causes tissues in our feet to stiffen and the range of motion and joint mobility to decrease, and we tend to put weight more on the inside of our feet—causing them to flatten and reduce the amount of force we have pushing forward when we walk. These are just some of the contributors to our propensity to experience foot pain and even increase our risk of falling as we get older. However there is hope. There are some exciting advancements in biomechanics—specifically footwear and orthotic devices—that can help improve foot health in older adults by adjusting gait and redistributing pressure away from certain areas of the foot which helps increase mobility and reduce pain. If you or someone you love is experiencing pain in the feet or reduced mobility, contact a podiatrist who may be able to help you feel and walk better.
As we age, biomechanics—the study of structure, function and movement—become more important to our foot health. Aging causes tissues in our feet to stiffen and the range of motion and joint mobility to decrease, and we tend to put weight more on the inside of our feet—causing them to flatten and reduce the amount of force we have pushing forward when we walk. These are just some of the contributors to our propensity to experience foot pain and even increase our risk of falling as we get older. However there is hope. There are some exciting advancements in biomechanics—specifically footwear and orthotic devices—that can help improve foot health in older adults by adjusting gait and redistributing pressure away from certain areas of the foot which helps increase mobility and reduce pain. If you or someone you love is experiencing pain in the feet or reduced mobility, contact a podiatrist who may be able to help you feel and walk better.
If you need your feet checked, contact Dr. Gary Cesar of Michigan Foot and Ankle Center. Our doctor will attend to all of your foot and ankle needs and provide you with quality treatment.
Geriatrics and Podiatry
When people age, some common issues that may occur are bone density loss, dry skin, poor circulation, and rough brittle nails. These issues may also affect your foot health if the necessary steps are not taken to alleviate the problems.
It is important to take care of your feet because feet that are injured or diseased can affect your overall health. Having painful feet hinders your ability to do daily activities or may decrease your willingness to do the things that you need to do.
Visiting Your Geriatrician
As we age, health problems become more likely, so it is essential to visit your doctor for check-ups to ensure that you are doing the best you can to take care of your health. It is recommended to check your feet frequently for any possible cuts, bruises, swelling, corns or any other irregularities.
Taking Care of Elderly Feet
Cracked or dry feet can be treated by applying moisturizer often. It is also important not to wear old socks because the older the sock is, the higher the possibility there will be that there is bacteria there. Wear fresh socks and make sure they fit properly.
Proper foot health means that you can have a more active lifestyle and you will not be bogged down by pain. Foot health also leads to good circulation, which is paramount for overall health.
If you have any questions, please feel free to contact our offices located in Lansing and Mt. Pleasant, MI . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Geriatrics and Podiatry
Bone density loss, dry skin, poor circulation, and rough and brittle nails are some of the common problems that can occur as people age. The effect that these problems has on foot health should be of particular concern in comprehensive geriatric care.
Feet that are diseased or injured have a negative effect on overall health and safety. Painful feet limit a person’s willingness and ability to stay active. Poor foot health can also cause gait change, which can lead to falls and accidents. Even though recovery time from health problems naturally slows as we age, many foot problems can be avoided altogether with regular prophylactic care.
Feet should be thoroughly washed in warm water daily. Care must be taken to dry the feet well, making sure to dry between and under the toes. Any left-over moisture can cause problems like foot fungus. After cleaning feet carefully check for problems such as cracked skin, bruises, swelling, cuts, corns, or other irregularities.
Examine toenails for ingrown, jagged, or split nails. Long toenails should be cut straight across. Never cut toenails at an angle or down the side as this may lead to ingrown nails.
Cracked and dry feet should be treated once or twice a day with a non-greasy moisturizer. Rub the moisturizer into the skin and allow it to dry before putting on socks and shoes. Sweaty feet can be dusted with a small amount of talcum powder. Avoid putting talcum directly into shoes as this may make feet slip within the shoe and cause a serious fall.
Wear clean dry socks each day. Not only do clean socks feel better on the feet, but socks worn for longer periods may harbor disease and odor-causing bacteria. Socks should not be tight around the top as they can leave marks on the leg. Socks that are too small can bring about bruising caused by pressure against the toes.
Wear comfortable and well-fitting shoes. If possible, consult a professional footwear specialist when purchasing shoes. Do not walk around barefoot as this exposes the feet to possible injury and bacteria.
Good foot health allows a more active lifestyle, which improves blood flow. Good circulation aids in recovery from injury or illness. It is also important for maintaining overall health.
Serious health problems can manifest themselves as symptoms in the feet. The elderly should seek professional help from a podiatrist if experiencing foot problems like tingling, numbness, pain, infection, or a sore that does not heal. Taking care of these problems right away can prevent the development of severe cases.
How Do Orthotics Work?
 Orthotics are specially designed shoe inserts that help correct imbalances and provide additional support to the feet. They can be purchased over the counter or be custom made by a podiatrist. Orthotics can help provide relief from a variety of conditions such as corns, calluses, ulcerations, tendonitis, heel pain, recurring stress fractures, and even hip and lower back pain. Since orthotics are designed to address specific problems, they can work in various ways that include relieving pressure by redistributing body weight or by providing extra shock absorption. Patients who believe that orthotics may help relieve their foot and ankle issues should consult with a podiatrist. A podiatrist looks at a variety of factors, such as the foot’s structure and function, biomechanics and lifestyle factors, to determine the right fit for each individual patient.
Orthotics are specially designed shoe inserts that help correct imbalances and provide additional support to the feet. They can be purchased over the counter or be custom made by a podiatrist. Orthotics can help provide relief from a variety of conditions such as corns, calluses, ulcerations, tendonitis, heel pain, recurring stress fractures, and even hip and lower back pain. Since orthotics are designed to address specific problems, they can work in various ways that include relieving pressure by redistributing body weight or by providing extra shock absorption. Patients who believe that orthotics may help relieve their foot and ankle issues should consult with a podiatrist. A podiatrist looks at a variety of factors, such as the foot’s structure and function, biomechanics and lifestyle factors, to determine the right fit for each individual patient.
If you are having discomfort in your feet and would like to try orthotics, contact Dr. Gary Cesar from Michigan Foot and Ankle Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Are Orthotics?
Orthotics are inserts you can place into your shoes to help with a variety of foot problems such as flat feet or foot pain. Orthotics provide relief and comfort for minor foot and heel pain but can’t correct serious biomechanical problems in your feet.
Over-the-Counter Inserts
Orthotics come in a wide variety of over-the-counter inserts that are used to treat foot pain, heel pain, and minor problems. For example, arch supports can be inserted into your shoes to help correct overarched or flat feet, while gel insoles are often used because they provide comfort and relief from foot and heel pain by alleviating pressure.
Prescription Orthotics
If over-the-counter inserts don’t work for you or if you have a more severe foot concern, it is possible to have your podiatrist prescribe custom orthotics. These high-quality inserts are designed to treat problems such as abnormal motion, plantar fasciitis, and severe forms of heel pain. They can even be used to help patients suffering from diabetes by treating foot ulcers and painful calluses and are usually molded to your feet individually, which allows them to provide full support and comfort.
If you are experiencing minor to severe foot or heel pain, it’s recommended to speak with your podiatrist about the possibilities of using orthotics. A podiatrist can determine which type of orthotic is right for you and allow you to take the first steps towards being pain-free.
If you have any questions please contact our offices located in Lansing and Mt. Pleasant, MI . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Foot Orthotics
Orthotics are shoe inserts that are meant to correct an irregular walking gait or provide cushioning to the feet. Orthotics come in a variety of different models and sizes, including over-the-counter and customizable variants. Customizable orthotics can be shaped and contoured to fit inside a specific shoe and are typically prescribed through a podiatrist who specializes in customized footwear and orthotics design and management.
Orthotics are beneficial because they can help prevent injuries from occurring and provide cushioning to keep pain levels down to a minimum. They also allow for the correct positioning of the feet. Orthotics can act as shock absorbers to help remove pressure from the foot and ankle. Therefore, orthotics can make bodily movements, such as walking and running, become more comfortable as well as help prevent the development of certain foot conditions.
Orthotics alleviate pain and make the foot more comfortable by slightly altering the angle at which the foot strikes the ground surface, therefore controlling the movement of the foot and ankle. Orthotics come in different variants and can be made of various materials. To determine what type of orthotic is most suited to your feet and your needs, it is best to consult your podiatrist. He or she will be able to recommend a type of orthotic that can help improve your foot function or prescribe a custom orthotic to best fit your feet.
Why Does My Big Toe Hurt?
 Big toe pain is often characterized by discomfort while walking, tenderness, swelling, bruising, discoloration, misalignment of the toe, and bumps or other disfigurements of the feet. The big toe can hurt for a variety of reasons. Injuries, such as a fracture, sprain, bruise, or dislocation of the toe can occur when the toe is struck by an object or stubbed. Nerve damage to the toe can be caused by Morton’s neuroma, a thickening of the nerve tissue in the foot in response to injury, irritation, or compression. Inflammatory conditions such as gout or rheumatoid arthritis can lead to joint pain. Bunions are also a common source of pain and disfigurement of the big toe. If you have pain in your big toe, please see a podiatrist for a proper diagnosis and treatment.
Big toe pain is often characterized by discomfort while walking, tenderness, swelling, bruising, discoloration, misalignment of the toe, and bumps or other disfigurements of the feet. The big toe can hurt for a variety of reasons. Injuries, such as a fracture, sprain, bruise, or dislocation of the toe can occur when the toe is struck by an object or stubbed. Nerve damage to the toe can be caused by Morton’s neuroma, a thickening of the nerve tissue in the foot in response to injury, irritation, or compression. Inflammatory conditions such as gout or rheumatoid arthritis can lead to joint pain. Bunions are also a common source of pain and disfigurement of the big toe. If you have pain in your big toe, please see a podiatrist for a proper diagnosis and treatment.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with Dr. Gary Cesar from Michigan Foot and Ankle Center. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our offices located in Lansing and Mt. Pleasant, MI . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot Pain
The feet, being the foundation of the body, carry all of the body’s weight and are therefore prone to experiencing pain and discomfort. If you are experiencing foot pain, it is important to determine where in the foot you are experiencing this pain to help discover the cause of it. While pain can be experienced virtually anywhere in the foot, the most common sites of foot pain are in the heel and ankle.
Heel pain can be due to a multitude of conditions including plantar fasciitis, Achilles tendinitis, and heel spurs. Pain experienced in the ankle can be a sign of an ankle sprain, arthritis, gout, ankle instability, ankle fracture, or nerve compression. In more serious cases, pain in the foot can be a sign of improper alignment or an infection.
Foot pain can be accompanied by symptoms including redness, swelling, stiffness and warmth in the affected area. Whether the pain can be described as sharp or dull depends on the foot condition behind it. It is important to visit your local podiatrist if your foot pain and its accompanying symptoms persist and do not improve over time.
Depending on the location and condition of your foot pain, your podiatrist may prescribe certain treatments. These treatments can include but are not limited to prescription or over-the-counter drugs and medications, certain therapies, cortisone injections, or surgery.
If you are experiencing persistent foot pain, it is important to consult with your foot and ankle doctor to determine the cause and location. He or she will then prescribe the best treatment for you. While milder cases of foot pain may respond well to rest and at-home treatments, more serious cases may take some time to fully recover.
Why Live with Pain and Numbness in Your Feet?
Who Is at Risk for Getting an Achilles Tendon Rupture?
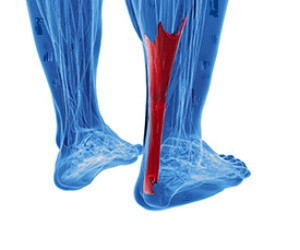
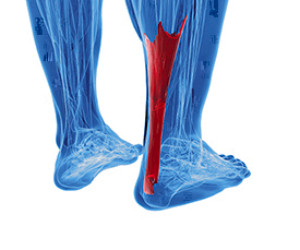 The large tendon on the back of the ankle connecting the calf muscle and the heel bone is known as the Achilles tendon. When this tendon tears, an Achilles tendon rupture may occur. A rupture is often common in sporting activities that involve pushing off the feet and sprinting, such as basketball and tennis. While Achilles tendon ruptures tend to happen more to males and people between the ages of 30 and 40, they can happen to anyone. Those who have poor flexibility, an inactive lifestyle, or are taking steroid medications may be at a higher risk for an Achilles tendon rupture as well. Signs of a rupture can include abrupt pain in the affected area, the feeling of getting kicked in the back of the leg, hearing a “pop” in back of the leg, weakness, and bruising or swelling in the area. If you believe that you have ruptured your Achilles tendon, or you would like to learn more about preventing a rupture, please consult with a podiatrist.
The large tendon on the back of the ankle connecting the calf muscle and the heel bone is known as the Achilles tendon. When this tendon tears, an Achilles tendon rupture may occur. A rupture is often common in sporting activities that involve pushing off the feet and sprinting, such as basketball and tennis. While Achilles tendon ruptures tend to happen more to males and people between the ages of 30 and 40, they can happen to anyone. Those who have poor flexibility, an inactive lifestyle, or are taking steroid medications may be at a higher risk for an Achilles tendon rupture as well. Signs of a rupture can include abrupt pain in the affected area, the feeling of getting kicked in the back of the leg, hearing a “pop” in back of the leg, weakness, and bruising or swelling in the area. If you believe that you have ruptured your Achilles tendon, or you would like to learn more about preventing a rupture, please consult with a podiatrist.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact Dr. Gary Cesar of Michigan Foot and Ankle Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our offices located in Lansing and Mt. Pleasant, MI . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Achilles Tendon Injuries
The Achilles tendon is the largest tendon in the body; it is a tough band of fibrous tissue that stretches from the bones of the heel to the calf muscles. This tendon is what allows us to stand on our toes while running, walking, or jumping, it is common for this tendon to become injured. In severe cases, the Achilles tendon may become partially torn or completely ruptured. However, this tendon is susceptible to injury because of its limited blood supply and the high level of tension it endures.
The people who are more likely to suffer from Achilles tendon injuries are athletes who partake in activities that require them to speed up, slow down, or pivot. Consequently, athletes who engage in running, gymnastics, dance, football, baseball, basketball, or tennis are more likely to suffer from Achilles tendon injuries. Additionally, there are other factors that may make you more prone to this injury. People who wear high heels, have flat feet, tight leg muscles or tendons, or take medicines called glucocorticoids are more likely to have Achilles tendon injuries.
A common symptom of an Achilles tendon injury is pain above the heel that is felt when you stand on your toes. However, if the tendon is ruptured, the pain will be severe, and the area may become swollen and stiff. Other symptoms may be reduced strength in the lower ankle or leg area, and reduced range of motion in the ankle. When the Achilles tendon tears, there is usually a popping sound that occurs along with it. People who have acute tears or ruptures may find walking and standing to be difficult.
If you suspect you have injured your Achilles tendon, you should see your podiatrist to have a physical examination. Your podiatrist will likely conduct a series of tests to diagnose your injury including a “calf-squeeze” test. Calf squeeze tests are performed by first squeezing the calf muscle on the healthy leg. This will pull on the tendon and consequently cause the foot to move. Afterward, the same test will be performed on the injured leg. If the tendon is torn, the foot won’t move because the calf muscle won’t be connected to the foot.