(517) 487-5171
Fax (517) 908-0172

Hyperhidrosis of the Feet
Hyperhidrosis of the feet, also termed plantar hyperhidrosis, is characterized by excessive sweating of the feet that can be onset by any cause, such as exercise, fever, or anxiety. Most people suffering from hyperhidrosis of the feet also experience hyperhidrosis of the hands, or palmar hyperhidrosis. Approximately 1-2% of Americans suffer from this disorder.
Sweating is a healthy process utilized by the body in order to cool itself and maintain a proper internal temperature, which is controlled by the sympathetic nervous system. In individuals with hyperhidrosis, the sympathetic nervous system works in "overdrive", producing far more sweat than is actually needed.
Plantar hyperhidrosis is considered primary hyperhidrosis. Secondary hyperhidrosis refers to excessive sweating that occurs in an area other than the feet, hands, or armpits, and this indicates that is related to another medical condition, such as menopause, hyperthyroidism, or Parkinson's disease.
Symptoms of hyperhidrosis of the feet can include foot odor, athlete's foot, infections, and blisters. Because of the continual moisture, shoes and socks can rot which creates an additional foul odor and can ruin the material, requiring shoes and socks to be replaced frequently. In addition to the physical symptoms, emotional health is often affected as this disorder can be very embarrassing.
If left untreated, hyperhidrosis will usually persist throughout an individual's life. However, there are several treatment options available. A common first approach to treating hyperhidrosis of the feet is a topical ointment. Aluminum chloride, an ingredient found in antiperspirants, can be effective at treating hyperhidrosis if used in high concentration and applied to the foot daily. Some individuals can experience relief this way, while others encounter extreme irritation and are unable to use the product. Another procedure is the use of Botulinum Toxin A, commonly referred to as Botox. This is injected directly into the foot, and is effective at minimizing the sweat glands in the injected area. These injections must be repeated every 4 to 9 months.
If these treatments are ineffective, oral prescription medications may be taken in an effort to alleviate the symptoms. Again, some will experience relief while others do not. Going barefoot reportedly provides relief for most sufferers.
A final approach to combating hyperhidrosis of the feet is through surgery. Surgery has been less successful on patients with plantar hyperhidrosis than on those with palmar hyperhidrosis. It is only recommended when sweating is severe and other treatments have failed to work. This kind of surgery usually involves going into the central nervous system, and cutting nerves to stop the transmission of signals telling the foot to sweat.
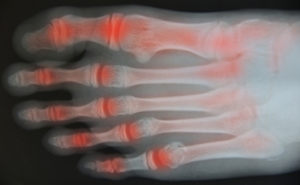
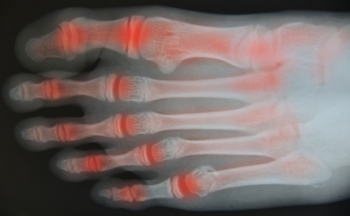
Symptoms of Psoriatic Arthritis in the Feet
Psoriatic arthritis (PsA) is a chronic autoimmune disease that affects the joints, including those on the feet. It typically affects people who have a skin condition called psoriasis. When PsA affects the feet, it produces symptoms such as painful toe swelling, joint stiffness, pain in the heels and soles of your feet, and dented or crumbling toenails. The condition has a pattern of flaring up and then subsiding. Your podiatrist can be an important part of your healthcare team when it comes to dealing with PsA in the feet. A podiatrist can help you find comfortable shoes and orthotics, maintain your mobility, and relieve symptoms during a flare up. To learn more, speak to a podiatrist today.
Arthritis can be a difficult condition to live with. If you are seeking treatment, contact Dr. Gary Cesar from Michigan Foot and Ankle Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
Arthritic Foot Care
Arthritis is a joint disorder that involves the inflammation of different joints in your body, such as those in your feet. Arthritis is often caused by a degenerative joint disease and causes mild to severe pain in all affected areas. In addition to this, swelling and stiffness in the affected joints can also be a common symptom of arthritis.
In many cases, wearing ill-fitting shoes can worsen the effects and pain of arthritis. Wearing shoes that have a lower heel and extra room can help your feet feel more comfortable. In cases of rheumatoid arthritis, the arch in your foot may become problematic. Buying shoes with proper arch support that contour to your feet can help immensely.
Alleviating Arthritic Pain
- Exercises that stretch the foot can prevent further pain and injury and increase mobility
- Most of the pain can be alleviated with anti-inflammatory drugs, heat, and topical medications
- Massages can help temporarily alleviate pain.
It is best to see your doctor for the treatment that is right for your needs and symptoms. Conditions vary, and a podiatrist can help you determine the right method of care for your feet.
If you have any questions, please feel free to contact our offices located in Lansing and Mt. Pleasant, MI . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Arthritic Foot Care
During your lifetime, you will probably walk about 75,000 miles, which is quite a lot of stress to put on your feet. As you get older, the 26 bones and 30 joints in each of your feet will lose flexibility and elasticity. Your foot’s natural shock absorbers will wear down as well. Having arthritis added to this mix only makes matters worse. Your joints will become distorted and inflamed, which is why arthritic foot care needs to be something to think about every day.
When dealing with arthritis, having additional foot complications, such as bunions, hammertoes, or neuroma, can be a serious detriment. To avoid these, buy well-fitting shoes with a lower heel and good support. Arthritis causes you to lose your arch, so having shoes with good arch support is also highly recommended.
Aside from getting good arch support, the shoes need to fit comfortably and properly as well. A good place to start is by leaving a finger width between the back of the shoe and your foot to gauge proper size. It is also helpful to have a square or rounded toe box in the front to provide even more comfort. Another thing to look for is a rubber sole that can provide a cushion and absorb shock as you walk. This adds flexibility to the ball of your foot when you push off your heel to walk.
Exercise is another key aspect of arthritic foot care. Exercise not only strengthens and stretches your muscles and joints, but helps to prevent further injury and pain as well. Stretching the Achilles tendon, the tendon located in the back of your heel, will give you added mobility and reduce pain due to stress. Another thing you can do is massage your feet, kneading the ball of your foot as well as your toes from top to bottom.
Stretching the Achilles tendon is a simple exercise that you can do at home anytime. Lean against the wall with your palms flat against the surface while placing one foot forward, towards the wall, and one foot behind you. Bend your forward knee towards the wall while keeping your back knee locked straight, and make sure both your heels are completely touching the ground at all times. This will stretch your Achilles tendon and calf muscles as well. You will feel the stretch almost immediately. You can also stretch your toes in a couple ways. One involves taking a rubber band and wrapping it around both your big toes while your heels remain together. Then, pull them apart to stretch your big toe. You can also place a rubber band around all the toes of one of your feet. Then, try to separate each individual toe, stretching them all.
A final step you can take to help your arthritis is taking non-steroid, non-inflammatory drugs or topical medicines with capsaicin. Unfortunately, there is no complete way to remove all of your arthritic pain. However, following some of this advice can go a long way in staying as pain-free as possible.
The Basics of Diabetic Foot Care
If you or someone you take care of has diabetes, there are a number of preventative practices that should be implemented to help keep your feet healthy and to avoid serious complications down the road. Shoes and socks should be worn during waking hours, even around the house. Check to make sure shoes fit properly and that there are no rough edges that will scrape against or cause a disturbance in the skin. Examine the feet daily. Early detection of any break in the skin will help avoid the injury from developing into a wound. Keep the feet clean and dry and the toenails trimmed straight across. Toenail length should be level with the tips of the toes, but not too short in order to prevent the nail from growing into the skin. Finally, any diabetic should be under the care of a podiatrist who can help them maintain proper foot health and manage any complications should they arise.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact Dr. Gary Cesar from Michigan Foot and Ankle Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our offices located in Lansing and Mt. Pleasant, MI . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Diabetic Foot Care
Diabetes can cause two problems that can potentially affect the feet: Diabetic neuropathy and Peripheral Vascular Disease. Diabetic neuropathy occurs when nerves in your legs and feet become damaged, which prevents you from feeling heat, cold, or pain. The problem with diabetic neuropathy is that a cut or sore on the foot may go unnoticed and the cut may eventually become infected. This condition is also a main cause of foot ulcers. Additionally, Peripheral vascular disease also affects blood flow in the body. Poor blood flow will cause sores and cuts to take longer to heal. Infections that don’t heal do to poor blood flow can potentially cause ulcers or gangrene.
There are certain foot problems that are more commonly found in people with diabetes such as Athlete’s foot, calluses, corns, blisters, bunions, foot ulcers, ingrown toenails, and plantar warts. These conditions can lead to infection and serious complications such as amputation. Fortunately, proper foot care can help prevent these foot problems before they progress into more serious complications.
Each day you should wash your feet in warm water with a mild soap. When you finish washing your feet, dry them carefully especially between your toes. You should also perform daily foot inspections to ensure you don’t have any redness, blisters, or calluses. Furthermore, if you are diabetic, you should always wear closed-toed shoes or slippers to protect your feet. Practicing these tips will help ensure that your feet are kept healthy and away from infection.
If you have diabetes, contact your podiatrist if you have any of the following symptoms on your feet: changes in skin color, corns or calluses, open sores that are slow to heal, unusual and persistent odor, or changes in skin temperature. Your podiatrist will do a thorough examination of your feet to help treat these problematic conditions.
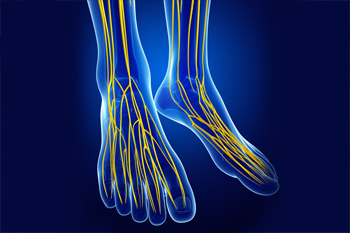
Posterior Tibial Nerve Neuralgia
Posterior tibial nerve neuralgia, also known as tarsal tunnel syndrome, is a nerve disorder that is caused by compression of the posterior tibial nerve. This nerve runs through the tarsal tunnel, an area along the inside of the ankle that houses nerves, blood vessels, and tendons. When the posterior tibial nerve is compressed, it causes symptoms such as foot, ankle, and toe pain, a pins and needles sensation in the foot, and numbness. Conservative treatments such as resting and icing the foot, wearing orthotics, and taking pain medications can help relieve symptoms. For more information about tarsal tunnel syndrome and to discover the best course of treatment for you, please consult with a podiatrist.
Tarsal tunnel syndrome can be very uncomfortable to live with. If you are experiencing tarsal tunnel syndrome, contact Dr. Gary Cesar of Michigan Foot and Ankle Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome, which can also be called tibial nerve dysfunction, is an uncommon condition of misfiring peripheral nerves in the foot. The tibial nerve is the peripheral nerve in the leg responsible for sensation and movement of the foot and calf muscles. In tarsal tunnel syndrome, the tibial nerve is damaged, causing problems with movement and feeling in the foot of the affected leg.
Common Cause of Tarsal Tunnel Syndrome
- Involves pressure or an injury, direct pressure on the tibial nerve for an extended period of time, sometimes caused by other body structures close by or near the knee.
- Diseases that damage nerves, including diabetes, may cause tarsal tunnel syndrome.
- At times, tarsal tunnel syndrome can appear without an obvious cause in some cases.
The Effects of Tarsal Tunnel Syndrome
- Different sensations, an afflicted person may experience pain, tingling, burning or other unusual sensations in the foot of the affected leg.
- The foot muscles, toes and ankle become weaker, and curling your toes or flexing your foot can become difficult.
- If condition worsens, infections and ulcers may develop on the foot that is experiencing the syndrome.
A physical exam of the leg can help identify the presence of tarsal tunnel syndrome. Medical tests, such as a nerve biopsy, are also used to diagnose the condition. Patients may receive physical therapy and prescriptive medication. In extreme cases, some may require surgery.
If you have any questions please feel free to contact our offices located in Lansing and Mt. Pleasant, MI . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Treating Tarsal Tunnel Syndrome
Tarsal tunnel syndrome is a condition in which the tibial nerve, located in the tarsal tunnel in the foot, is compressed. The tibial nerve can become compressed from injury, such as an ankle sprain, flat feet, and lesions. Arthritis, diabetes, and varicose veins can also cause swelling and thus result in nerve compression.
Symptoms of tarsal tunnel syndrome include several different sensations in the sole of the foot, inside the ankle, and around the tibial nerve. These sensations include shooting pains, numbness or reduced sensation, pins and needles, burning, and tingling. Symptoms tend to worsen with greater activity to the area. In rare and severe occasions, this can change the muscles in the foot.
If you suspect you have tarsal tunnel syndrome, you should consult with your podiatrist. He or she will examine your medical history to see if you have a history of diabetes, arthritis, or flat feet. They will also check to see if you have suffered an injury to the area recently. An electrical test will be conducted to check if the nerve has been damaged. A simpler Tinel’s Test might also be used. This includes simply tapping the nerve to create a sensation. An MRI scan of the area may also be used.
Treatments vary greatly for tarsal tunnel syndrome. Treatments include both nonsurgical and surgical options depending upon the severity of the condition. Nonsurgical options include anti-inflammatory medication and steroid injections to the area. Orthotics, such as a splint or brace that immobilizes the foot, is another noninvasive option. For those with flat feet, custom shoes can be made to offer better foot support. Surgical options include a tunnel tarsal release, in which an incision is made behind the ankle down to the arch of the foot. This releases the ligament and relieves pressure off the nerve. Some doctors use a more minimally invasive surgery, where smaller incisions are made in the ankle and the ligament is stretched out.
If you are suffering from painful sensations in your foot, see a podiatrist who can determine if you are experiencing tarsal tunnel syndrome. Tarsal tunnel syndrome that is left unchecked can cause permanent nerve damage to the foot.
Did I Break My Foot?
 There are 26 bones in the foot, which means that there are a variety of complex ways the foot can be fractured. These types of fractures can include toe fractures, midfoot fractures (metatarsal fractures), sesamoid fractures, or fractures to the bones at the back of the foot (e.g., the heel bone). If a foot is fractured, it will be very painful, and putting weight on it or walking will likely be difficult. If you believe that you have broken your foot, consulting with a podiatrist is suggested because you may need X-rays to confirm the fracture and a professional will be able to determine the best treatment options for you. Common treatment options for a broken foot include splints, casts, physical therapy, and keeping weight off of it.
There are 26 bones in the foot, which means that there are a variety of complex ways the foot can be fractured. These types of fractures can include toe fractures, midfoot fractures (metatarsal fractures), sesamoid fractures, or fractures to the bones at the back of the foot (e.g., the heel bone). If a foot is fractured, it will be very painful, and putting weight on it or walking will likely be difficult. If you believe that you have broken your foot, consulting with a podiatrist is suggested because you may need X-rays to confirm the fracture and a professional will be able to determine the best treatment options for you. Common treatment options for a broken foot include splints, casts, physical therapy, and keeping weight off of it.
A broken foot requires immediate medical attention and treatment. If you need your feet checked, contact Dr. Gary Cesar from Michigan Foot and Ankle Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
Broken Foot Causes, Symptoms, and Treatment
A broken foot is caused by one of the bones in the foot typically breaking when bended, crushed, or stretched beyond its natural capabilities. Usually the location of the fracture indicates how the break occurred, whether it was through an object, fall, or any other type of injury.
Common Symptoms of Broken Feet:
- Bruising
- Pain
- Redness
- Swelling
- Blue in color
- Numbness
- Cold
- Misshapen
- Cuts
- Deformities
Those that suspect they have a broken foot shoot seek urgent medical attention where a medical professional could diagnose the severity.
Treatment for broken bones varies depending on the cause, severity and location. Some will require the use of splints, casts or crutches while others could even involve surgery to repair the broken bones. Personal care includes the use of ice and keeping the foot stabilized and elevated.
If you have any questions please feel free to contact our offices located in Lansing and Mt. Pleasant, MI . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Causes, Symptoms, and Treatment for a Broken Foot
One out of ten broken bones is reported to be in the feet. When an object crushes, bends, or stretches the bone beyond acceptable ranges, bones break. A break in the foot is either a fracture or a straight break.
The location of any break can tell you how the break happened. Toes, for instance, break typically as a result of something being kicked hard and with great force. Heel breaks almost always are a result of an improper landing from a tall height. Twists or sprains are the other two frequent occurrences. As with all usual breaks, they result from unexpected accident or sudden injury. As with stress fractures, breaks form as a process over time from repeated stress on already present cracks. Runners, dancers, and gymnasts are the usual athletes who receive this type of break. Stress fractures result from incredible pressure on the feet. It is no surprise these athletes bear the majority of reported fractures.
Pain, swelling, bruising, and redness are all indicative of the typical symptoms from a broken foot. Severe pain—to the point of not being able to walk—usually depends on the location of the break in the foot. Toes are on the lower scale of pain threshold, but heels are high, as are a few other particular bones. As the severity of the broken foot increases, symptoms like blueness, numbness, misshaping of the foot, cuts, or deformities will become apparent. These symptoms indicate the need to see a medical professional with access to an x-ray facility.
Prior to seeing a specialist, precautions should be taken to reduce pain and swelling. Elevate and stabilize the foot, and refrain from moving it. Immobilization of the foot is the next priority, so creating a homemade splint is acceptable. Keep in mind that while creating a splint, any increase of pain or cutting off blood circulation means that the splint should be removed immediately. Use ice to decrease swelling and relieve pain symptoms.
When dealing with a medical center, the patient should note that the treatment can vary. The treatment will depend on the severity of the fracture and the cause of the break. Crutches, splits, or casts are common treatments while surgery has been known to be used in more severe cases in order to repair the break in the bones.